False-Positive COVID-19 Results: Hidden Problems and Costs
The Lancet Volume 8, ISSUE 12, P1167-1168, December 01, 2020
False-positive COVID-19 results: hidden problems and costs
Published: September 29, 2020, DOI:https://doi.org/10.1016/S2213-2600(20)30453-7
RT-PCR tests to detect severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA are the operational gold standard for detecting COVID-19 disease in clinical practice. RT-PCR assays in the UK have analytical sensitivity and specificity of greater than 95%, but no single gold standard assay exists.1 , 2 New assays are verified across panels of material, confirmed as COVID-19 by multiple testing with other assays, together with a consistent clinical and radiological picture. These new assays are often tested under idealised conditions with hospital samples containing higher viral loads than those from asymptomatic individuals living in the community. As such, diagnostic or operational performance of swab tests in the real world might differ substantially from the analytical sensitivity and specificity.2
Although testing capacity and therefore the rate of testing in the UK and worldwide has continued to increase, more and more asymptomatic individuals have undergone testing. This growing inclusion of asymptomatic people affects the other key parameter of testing, the pretest probability, which underpins the veracity of the testing strategy. In March and early April, 2020, most people tested in the UK were severely ill patients admitted to hospitals with a high probability of infection. Since then, the number of COVID-19-related hospital admissions has decreased markedly from more than 3000 per day at the peak of the first wave, to just more than 100 in August, while the number of daily tests jumped from 11 896 on April 1, 2020, to 190 220 on Aug 1, 2020. In other words, the pretest probability will have steadily decreased as the proportion of asymptomatic cases screened increased against a background of physical distancing, lockdown, cleaning, and masks, which have reduced viral transmission to the general population. At present, only about a third of swab tests are done in those with clinical needs or in health-care workers (defined as the pillar 1 community in the UK), while the majority are done in wider community settings (pillar 2). At the end of July, 2020, the positivity rate of swab tests within both pillar 1 (1·7%) and pillar 2 (0·5%) remained significantly lower than those in early April, when positivity rates reached 50%.3
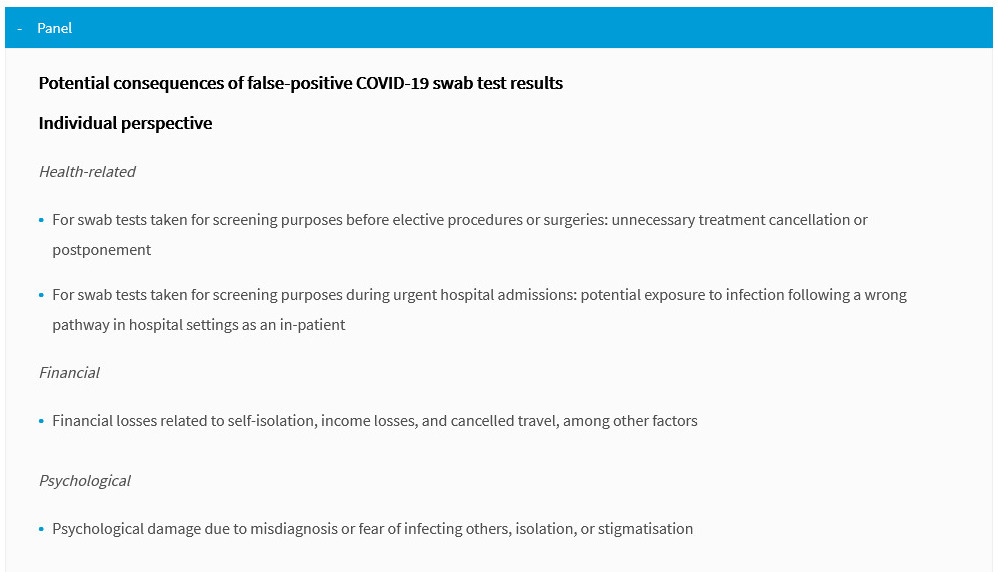
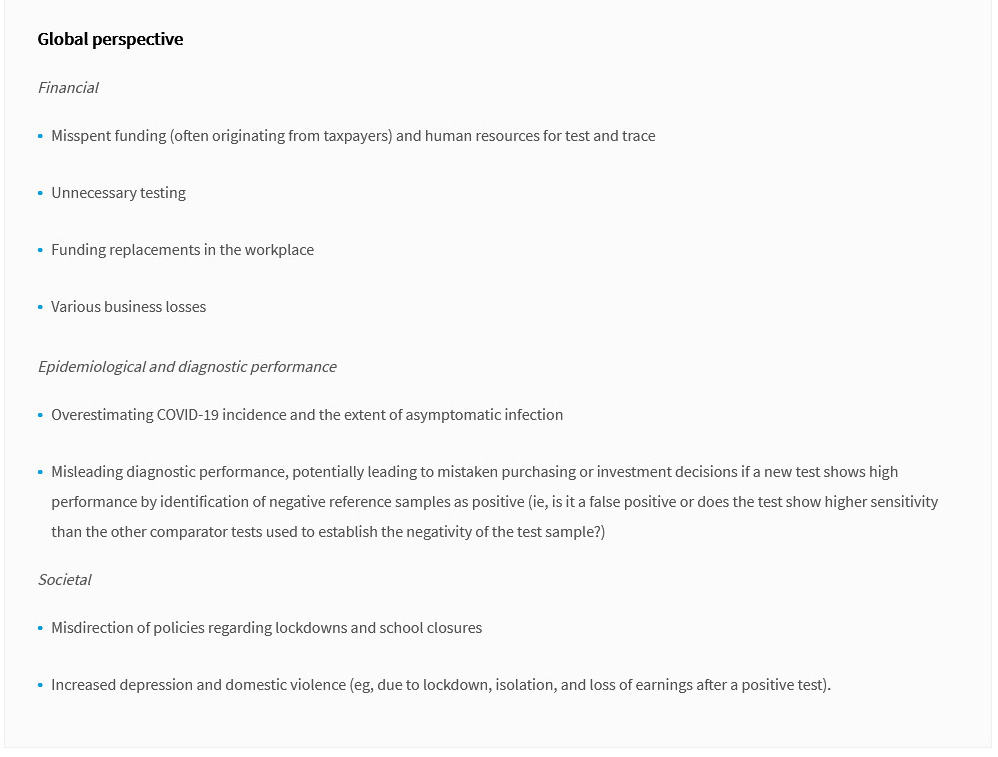
Globally, most effort so far has been invested in turnaround times and low test sensitivity (ie, false negatives); one systematic review reported false-negative rates of between 2% and 33% in repeat sample testing.4 Although false-negative tests have until now had priority due to the devastating consequences of undetected cases in health-care and social care settings, and the propagation of the epidemic especially by asymptomatic or mildly symptomatic patients,1 the consequences of a false-positive result are not benign from various perspectives (panel), in particular among health-care workers.
Technical problems including contamination during sampling (eg, a swab accidentally touches a contaminated glove or surface), contamination by PCR amplicons, contamination of reagents, sample cross-contamination, and cross-reactions with other viruses or genetic material could also be responsible for false-positive results.2 These problems are not only theoretical; the US Center for Disease Control and Prevention had to withdraw testing kits in March, 2020, when they were shown to have a high rate of false-positives due to reagent contamination.5
The current rate of operational false-positive swab tests in the UK is unknown; preliminary estimates show it could be somewhere between 0·8% and 4·0%.2 , 6 This rate could translate into a significant proportion of false-positive results daily due to the current low prevalence of the virus in the UK population, adversely affecting the positive predictive value of the test.2 Considering that the UK National Health Service employs 1·1 million health-care workers, many of whom have been exposed to COVID-19 at the peak of the first wave, the potential disruption to health and social services due to false positives could be considerable.
Any diagnostic test result should be interpreted in the context of the pretest probability of disease. For COVID-19, the pretest probability assessment includes symptoms, previous medical history of COVID-19 or presence of antibodies, any potential exposure to COVID-19, and likelihood of an alternative diagnosis.1 When low pretest probability exists, positive results should be interpreted with caution and a second specimen tested for confirmation. Notably, current policies in the UK and globally do not include special provisions for those who test positive despite being asymptomatic and having laboratory confirmed COVID-19 in the past (by RT-PCR swab test or antibodies). Prolonged viral RNA shedding, which is known to last for weeks after recovery, can be a potential reason for positive swab tests in those previously exposed to SARS-CoV-2. However, importantly, no data suggests that detection of low levels of viral RNA by RT-PCR equates with infectivity unless infectious virus particles have been confirmed with laboratory culture-based methods.7 If viral load is low, it might need to be taken into account when assessing the validity of the result.8
To summarise, false-positive COVID-19 swab test results might be increasingly likely in the current epidemiological climate in the UK, with substantial consequences at the personal, health system, and societal levels (panel). Several measures might help to minimise false-positive results and mitigate possible consequences. Firstly, stricter standards should be imposed in laboratory testing. This includes the development and implementation of external quality assessment schemes and internal quality systems, such as automatic blinded replication of a small number of tests for performance monitoring to ensure false-positive and false-negative rates remain low, and to permit withdrawal of a malfunctioning test at the earliest possibility. Secondly, pretest probability assessments should be considered, and clear evidence-based guidelines on interpretation of test results developed. Thirdly, policies regarding the testing and prevention of virus transmission in health-care workers might need adjustments, with an immediate second test implemented for any health-care worker testing positive. Finally, research is urgently required into the clinical and epidemiological significance of prolonged virus shedding and the role of people recovering from COVID-19 in disease transmission.